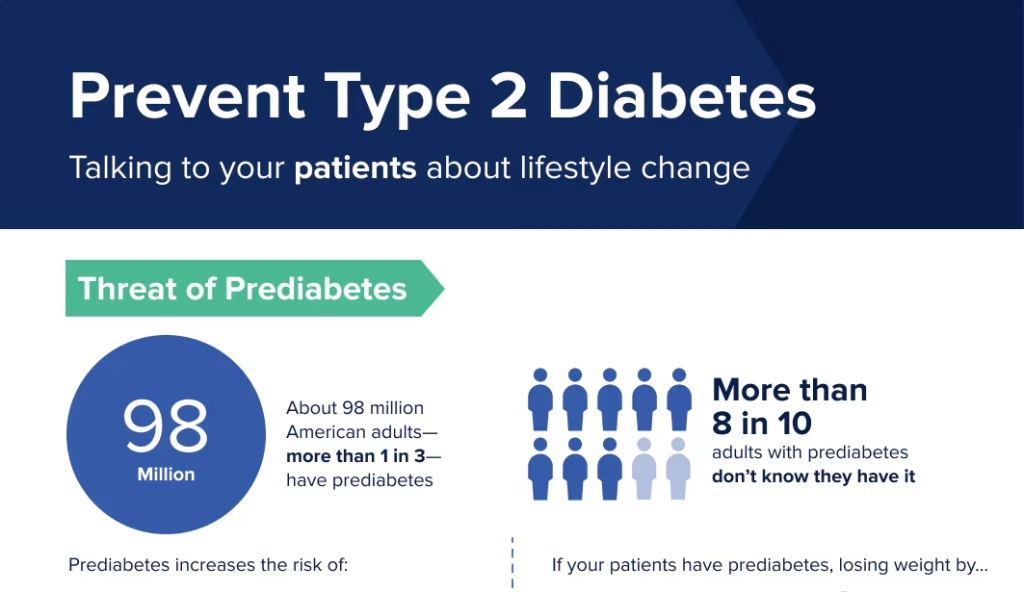
The statistics are overwhelming and, frankly, unacceptable. According to the American Diabetes Association (ADA), more than 37 million Americans are living with diabetes, with diagnosed Type 2 diabetes accounting for most of these cases. Also concerning is that 96 million American adults have prediabetes, and most of these people are unaware of their risks. This is a bubbling public health crisis and a looming economic catastrophe.
According to the ADA, the diagnosed cost of diabetes in the United States is estimated to be $412.9 billion in 2022, including both direct medical costs and indirect costs like lost productivity. As the prevalence of diabetes continues to rise, costs will climb higher and higher, placing an unsustainable and unnecessary burden on our health system and economy. It points to a stark, uncomfortable realization that the biggest cost burden on the American taxpayer isn’t drugs (11 percent of the total national health spend); it is the cost of manageable disease run amuck.
While the White House and Congress rightly tout their success in lowering the cost of insulin for Americans in need, the policy victory speaks to the persistent problem—akin to closing the barn door after the horse has escaped—that more and more people are being diagnosed with or unaware of their diabetes risks. The bigger “hairy audacious goal” is to reduce the number of people with diabetes in the first place.
A Tale of Two Americas
The Type 2 diabetes epidemic is not an equal opportunity offender. It disproportionately affects racial and ethnic minorities, as well as those with lower educational attainment and socioeconomic status. This is not a coincidence; it results from systemic inequalities plaguing our health-delivery system. It speaks to the long overdue need to use PK-12 education to inform young people about healthy diets.
Black Americans, Hispanic/Latino Americans, and Native Americans bear a heavier burden of this disease because of deeply rooted social determinants of health. Access to quality healthcare, education, and economic opportunities are crucial in determining who develops Type 2 diabetes and who doesn’t.
According to the ADA: “The poorer you are in America, the less likely you are to have a grocery store within walking distance of your home. Diabetes rates are inversely related to income level, and nutrition is critical to diabetes prevention and management. Every American with diabetes and prediabetes must have access to affordable, culturally relevant food and the information they require to eat healthfully.”
At the heart of this crisis lies a fundamental issue raised for years: our relationship with food and education. The lack of basic nutritional literacy in many communities is not just unfortunate; it’s a tipping point for heart disease and diabetes. Many Americans, particularly in underserved communities, make food choices that harm their health because of strained household economics or lack of information. The food label on packaged goods is helpful to those who can translate the percentages listed into actionable decisions. Still, desperation often makes those decisions for people regardless of what the label says.
In urban and rural areas with limited access to fresh, nutritious food, food deserts are not just inconveniences but public health hazards. When the only food options available are processed, high-calorie, or convenient and tasty fast foods, we set up communities for a lifetime of health struggles.
Innovation and Public Policy: Islands of Hope
Traditional approaches are proving inadequate in the face of this growing threat. The health system needs to embrace innovative, policy- and technology-driven solutions that can reach people where they are and provide personalized support.
More than 41 million people participate in the Supplemental Nutrition Assistance Program (SNAP) and receive an average monthly benefit of $191 per person, or a little over $2 per meal. Roughly four out of 10 SNAP participants (42%) are children under age 18; 16% are people 60 and older, and about 12% are people with disabilities. The results are dramatic!
Children receiving SNAP benefits have better health status than youngsters who are not SNAP participants, and their households are less likely to sacrifice health care to pay for other necessary expenses. Older SNAP participants are less likely to be admitted to a nursing home or hospital than their counterparts who do not participate. It seems like common sense. Caring for the chronically ill costs taxpayers more.
Telemedicine and remote monitoring technologies offer potential avenues for diabetes management. These tools can provide real-time data to healthcare providers, allowing for more timely interventions and personalized care plans. AI-powered nutritional guidance apps have the potential to democratize access to customized meal plans, accounting for an individual’s health status, cultural preferences, and economic constraints. These tech tools can only be used as preventive and interventional extensions of the doctor’s office if third-party payers – private and public – ensure it is in the health providers’ interests.
On the pharmaceutical side of innovation are the GLP-1 receptors – that can help millions of people struggling with obesity – among the key catalysts for the surge in pre- and Type 2 diabetes. GLP-1 receptor agonists mimic the hormone’s action, crucial in regulating blood sugar levels. But here’s the kicker: these drugs don’t just lower blood glucose; they’re a Swiss Army knife of metabolic health. However, private payers often place obstacles in the path of access. Obesity is a complex – tipping point – disease leading to diabetes, mental health challenges, heart disease, and more. Payers often will not authorize GLP-1 use for people who are overweight and have prediabetes – waiting till people (their beneficiaries) graduate to Type 2, citing cost.
The Obesity Society spokesperson Katherine H. Saunders, MD, of Weill Cornell Medicine, New York City, in an interview with Medscape, comments: “What is more expensive than Wegovy (a GLP-1 class drug)? A day in the hospital. This is a particularly important finding for health plans, employers, and any group covering the total cost of care — many of whom are concerned about the cost of Wegovy. Hopefully, this data will encourage more decision makers to recognize not only the significant health benefits associated with Wegovy but also potential cost savings.” Dr. Saunders is among the nation’s top thinkers in the field of obesity and associated conditions, and as an entrepreneur, co-founded FlyteHealth, a community of health providers who specialize in helping people manage their weight.
Health- or Sick-Care – We Must Choose a Path
The economic impact of Type 2 diabetes is staggering. The time for half-measures and incremental change is long past. We need a coordinated, multisectoral response—the health sector, industry, government, and private philanthropy—working together to address the epidemic’s foundational causes.
Five suggestions include:
- Investing in education at the primary school level and ensuring children understand healthy food choices and have access to in-school meals.
- Addressing social determinants of health through Federal and state policies that promote economic equity and access to quality health and education
- Leveraging well-proven approaches in remote patient monitoring to improve diabetes intervention, detection, and management
- Strengthening the use of Federal and state programs such as SNAP and the Child and Adult Care Food Program (CACFP)
- Fostering collaboration between health providers, community organizations, national professional health organizations and tech companies to deploy proven solutions.

The Future We Must Embrace
Current efforts to address Type 2 and prediabetes prevention are insufficient. By acknowledging the complex relationship among social, educational, economic, and environmental factors contributing to this chronic illness epidemic, the United States private and public health system must examine drug costs; however, it can develop more effective policies and campaigns for diabetes intervention and management.
It’s time for a mindset shift in approaching this preventable condition. We must recognize that we have, to date, given lip service and window dressing to address disparities and support the needs of children growing up without sufficient knowledge about food choices or, in the case of cash-strapped families, access to a healthy meal that reinforces what they are learning in school. Half measures were never good enough and are no longer acceptable.
Every step toward managing Type 2 diabetes – or better yet, preventing it entirely – is a step toward a healthier, more equitable society. The challenge is immense, but the ability to make a difference is possible. There are proven delivery methods for insulin, vastly improved ways to monitor blood glucose and policies that could be tweaked to meet people’s needs. Together, we can turn the tide on this epidemic and create a future where Type 2 diabetes is no longer a looming threat but a manageable condition.
Pay now or pay later. It’s a decision payers and policymakers must make.



